Microflare Protocol Using Microdose Lupron (“short” protocol)
Details about the microflare ovarian stimulation protocol for IVF poor responders
To maximize success with in vitro fertilization we try to get multiple eggs to develop
- We prefer to get about 10-15 high-quality eggs at the egg retrieval procedure
- IVF success rates correlate with the number of eggs retrieved with IVF
However, some women are low responders to the ovarian stimulating drugs.
- They might develop a low number of follicles after being stimulated with high doses of IVF medications
- To improve chances for success, these women should be treated with specific IVF protocols
How many follicles do you need in order to get pregnant with IVF?
Usually, it is not difficult to get enough follicles to develop. However, women with low ovarian reserve often have a poor response to stimulation – and a low number of growing follicles are seen.
- The ability of the ovaries to stimulate and make numerous follicles can be predicted by an ultrasound test – the antral follicle count, and other ovarian reserve tests.
The minimum number of follicles needed to proceed with IVF treatment depends on several factors, including follicle sizes, age of the woman, results of previous IVF stimulations and the willingness of the couple (and the fertility doctor) to proceed with egg retrieval when a very low number of eggs will be obtained.
In our experience, IVF success rates are extremely low with less than 3 mature follicles
When the response of the ovaries to the stimulation attempt is insufficient – the IVF cycle is canceled, and often the couple will “convert” the cycle to intrauterine insemination, IUI.
More about IVF cycle cancellation
Women that are more likely to be low responders to ovarian stimulation would be those that have low antral follicle counts, those women who are older than about 37, women with elevated FSH levels, or low AMH levels, and women with other signs of reduced ovarian reserve.
We try to stimulate the woman to get a minimum of 3 follicles with a size of 14-18 mm in diameter with a flare stimulation. Ideally, there would be 6-8 or more follicles in that size range and more that are somewhat smaller. The goal is to get an ideal number of good quality eggs to work with.
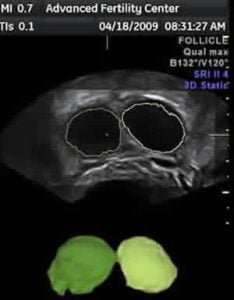
Views of two follicles in an ovary with a low response to stimulation
A 2D plane is shown at the top, 3D view at the bottom
The green follicle measured 19 mm diameter
The yellowish one was 18 mm
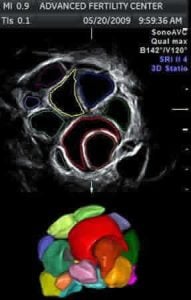
Views of multiple follicles – ovary with a good response to stimulation
A 2D plane is shown at top, a 3D view at the bottom
Stop Lupron Protocol for Low Responders
Some women are “over-suppressed” by the standard long Lupron protocol, or are low responders for some other reason. A “stop Lupron” protocol is one option for trying to get a better response to stimulation. The “flare-up” protocols are another option.
With a stop-Lupron protocol, it is started at the same time in the cycle as with the luteal Lupron protocol, but usually at a lower dose, such as at 5 units daily instead of 10 or 20 units. It is then stopped completely after the woman gets her period and the FSH product is started.
The LH suppressing ability of this protocol is not as complete as with the standard “long” Lupron protocol. However, the risk for a premature LH surge is low, and blood tests can be done during the cycle to watch for an LH surge.
Flare Protocol, or Microflare for Poor Response Cases (also called Microdose flare, short Lupron, or short protocol)
We are trying to take advantage of an initial “flare-up” response of FSH and LH release from the woman’s own pituitary gland that usually occurs in the first 3 days of agonist administration. Continuing Lupron for more than 3 days temporarily suppresses the pituitary gland so that it has a low output of FSH and LH.
The FSH product (e.g. Follistim, Gonal-F) is started on the following day (day 3). The idea is that Lupron will stimulate release of a large amount of FSH (and LH) that will jump-start (flare-up) the follicles so that we might have a better ovarian stimulation with more mature follicles and more eggs for IVF.
The FSH product (e.g. Follistim, Gonal-F) is started on the following day (day 3). The idea is that Lupron will stimulate release of a large amount of FSH (and LH) that will jump-start (flare-up) the follicles so that we might have a better ovarian stimulation with more mature follicles and more eggs for IVF.
Birth control pills are usually given for the month before the flare so that there will not be a leftover cyst (corpus luteum) that could become reactivated by the high LH levels at the onset of the flare stimulation.
An example of a microflare protocol is given below – there are variations on the theme:
- Birth control pills for 1 month
- Stop birth control pills – no meds for 2 days
- Start Lupron on the third pill free day. We use a 50ug dose twice daily – AM and PM – for these flare cycles. 50ug is a very small dose as compared to the usual Long Lupron protocol dose of 0.5mg (500ug). The Lupron must be diluted by the pharmacy or the doctor’s office to be able to inject such a low dose.
- Start injections of the FSH product (once or twice daily) on the day after starting Lupron
- The Lupron is usually continued at the same dose until the HCG trigger shot is given.
- Some fertility specialists believe that lead follicle sizes with a flare stimulation should not be greater than about 17-19mm – or pregnancy success rates may be reduced.
Some women do not respond well to a flare protocol (or any other protocol) and will not be able to develop enough follicles to allow a reasonable chance for pregnancy from IVF with their own eggs. These women are good candidates for IVF with donor eggs.
Some fertility specialists believe that women who are low responders might stimulate better if an antagonist protocol (Ganirelix or Cetrotide) is used.
Sample calendar for Microdose flare for IVF
Overview about ovarian stimulation for IVF
Details about antagonist IVF protocols – using Ganirelix or Cetrotide
Details about the long Lupron protocol – also called down regulation