Ovarian reserve, which includes the number of antral follicles, is an important indicator of a woman's egg supply. Testing ovarian reserve helps predict how the ovaries will respond to stimulation during fertility treatments.
Background
Women are born with all the eggs they will ever have. Eggs are lost constantly until menopause, when none remain. “Ovarian reserve” refers to the reserve of the ovaries (remaining egg supply) to be able to make babies. We want a test that shows how many eggs a woman has at a point in time – as well as telling us about the quality of the eggs. Antral follicle counts by ultrasound are one of the best ovarian reserve tests that we currently have available.
What are Antral Follicles?
Antral follicles are small follicles (about 2-9 mm in diameter) that we can see – and measure and count – with ultrasound. Antral follicles are also referred to as resting follicles. Vaginal ultrasound is the best way to accurately assess and count these small structures. Antral follicle counts (along with female age) are by far the best tool that we currently have for estimating ovarian reserve, the expected response to ovarian stimulating drugs, and the chance for successful pregnancy with in vitro fertilization. The number of antral follicles visible on ultrasound is indicative of the number of microscopic (and sound asleep) primordial follicles remaining in the ovary. Each primordial follicle contains an immature egg that can potentially develop and ovulate in the future. When there are only a few antral follicles visible, there are far fewer eggs remaining as compared to when there are more antrals. As women age, they have less eggs (primordial follicles) remaining and they have fewer antral follicles. Antral follicle counts are a good predictor of the number of mature follicles that we will be able to stimulate in the woman’s ovaries when we give injectable FSH medications that are used for in vitro fertilization. The number of eggs retrieved correlates with IVF success rates.
- When there are an average (or high) number of antral follicles, we tend to get a “good” response with many mature follicles. We tend to get a good number of eggs at retrieval in these cases. Pregnancy rates are higher than average.
- When there are few antral follicles, we tend to get a poor response with few mature follicles. Cancellation of an IVF cycle is much more common when there is a low antral count. Pregnancy rates are lower overall in this group. The reduction in success rates is more pronounced in women over 35 years old.
- When the number of antral follicles is intermediate, the response is not as predictable. In most cases the response is intermediate. However, we could also have either a low or a good response when the antral counts are intermediate. Pregnancy rates are pretty good overall in this group.
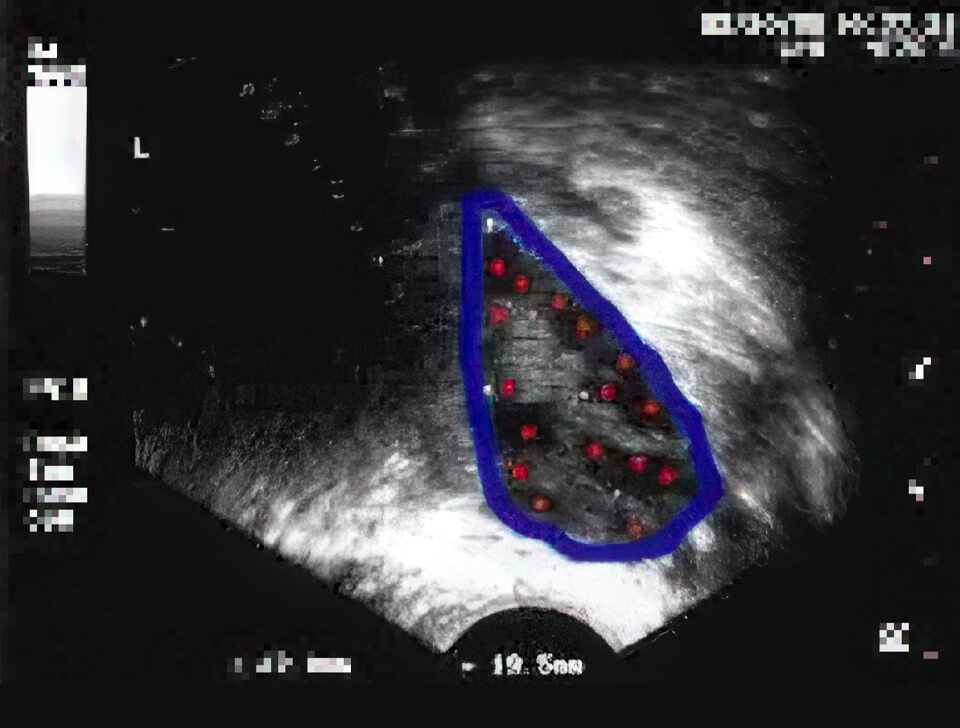
High ovarian volume and high antral follicle counts
Ultrasound image of an ovary at the beginning of a menstrual cycle. No medications being given. The ovary is outlined in blue. There are numerous antral follicles visible – marked with red. 16 are seen in this image. Ovary had a total of 35 antrals (only 1 plane is shown). This is a polycystic ovary, with a high antral count and high volume (ovary = 37 by 19.5mm) This woman had irregular periods and was a “high responder” to injectable FSH drugs.
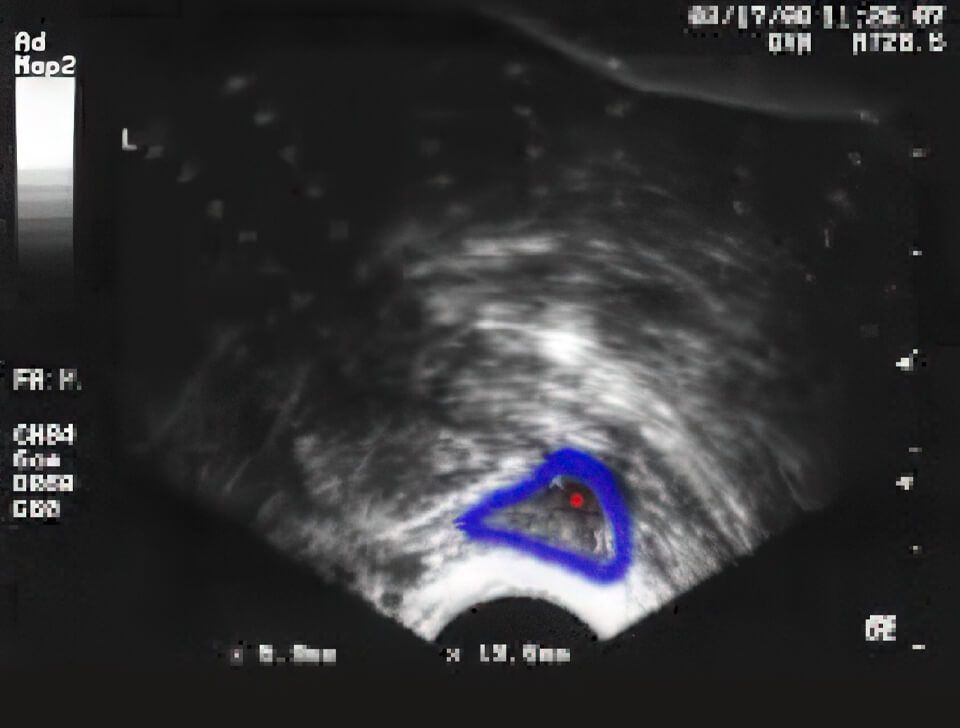
Normal ovarian volume and “normal” antral follicle counts
Ultrasound image of an ovary early in the menstrual cycle. No medications being given. The ovary is outlined in blue. 9 antral follicles are seen – marked with red. The ovary has normal volume (cursors measuring ovary = 30 by 18mm). Expect a normal response to injectable FSH.
Low ovarian volume and low antral follicle counts
An ovary is outlined in blue and is small (low volume) with only 1 antral Her other ovary had only 2 antrals She had regular periods and a normal day 3 FSH test Attempts to stimulate her “sleepy” ovaries for IVF were not successful.
How many antral follicles is “good”?
There is not a perfect answer to this question. Unfortunately, we do not live in a perfect world, and some ovaries have not yet read up on antral follicle counts to know how they are supposed to respond to stimulation. Antral follicle counts can also be somewhat “observer-dependent”. This means that if we had several different trained ultrasonographers do an antral count on a woman, they would not all get exactly the same result. Therefore, what we decide looks like 6 antral follicles, at another clinic might have been read as 4 or 8, etc.
From our own observations and experience, here are some general guidelines:
| Total number of antral follicles | Expected response to injectable stimulating drugs and chances for IVF success |
| Less than 4 | Extremely low count, very poor (or no) response to stimulation is expected. Cycle cancellation is likely. Possibly should consider not attempting IVF at all. |
| 4-9 | Low count, we are concerned about a possible/probable poor response to the stimulation drugs. Likely to need high doses of FSH product to stimulate ovaries adequately. Higher than average rate of IVF cycle cancellation. Lower than average pregnancy rates for those cases that make it to egg retrieval. |
| 9-13 | Somewhat reduced count Higher than average rate of IVF cycle cancellation. Slight to moderate reduction in chances for pregnancy success as a group. |
| 14-21 | Intermediate (and “normal”) count Response to drug stimulation is sometimes low, but is usually good. Pregnancy rates as a group are slightly reduced compared to the “best” group. |
| 22-35 | Normal (good) antral count, should have an excellent response to ovarian stimulation. Likely to respond well to low doses of FSH drugs. Very low risk for IVF cycle cancellation. Some risk for ovarian overstimulation if a Lupron trigger is not used for final egg maturation injection. Excellent pregnancy success rates. |
| Over 35 | Very high count, watch for polycystic ovary type of ovarian response. Likely to have a high response to low doses of FSH product. Higher risk for overstimulation and ovarian hyperstimulation syndrome if a Lupron trigger is not utilized. Very good pregnancy rate overall. |
Correlation of antral counts and IVF outcomes
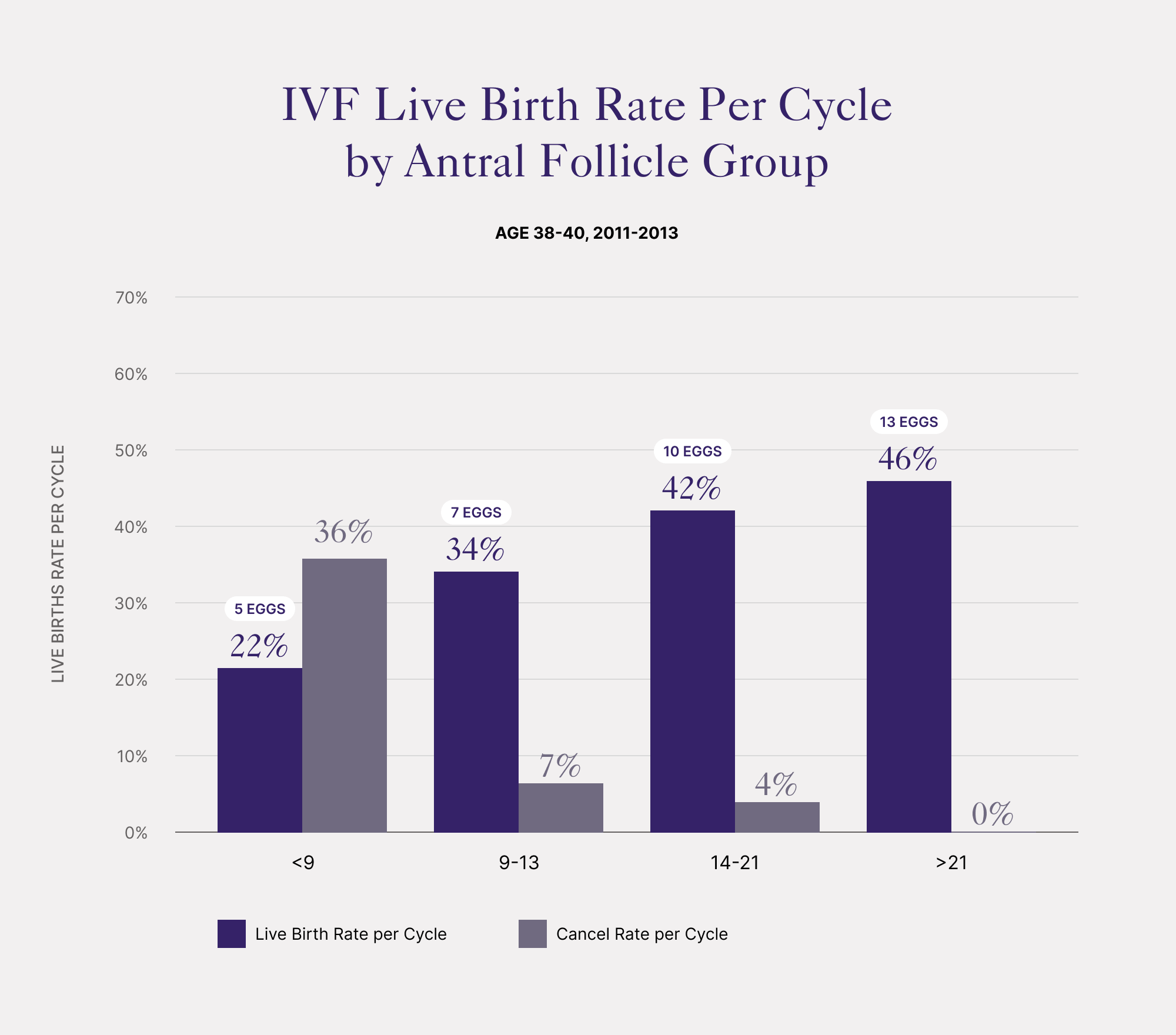
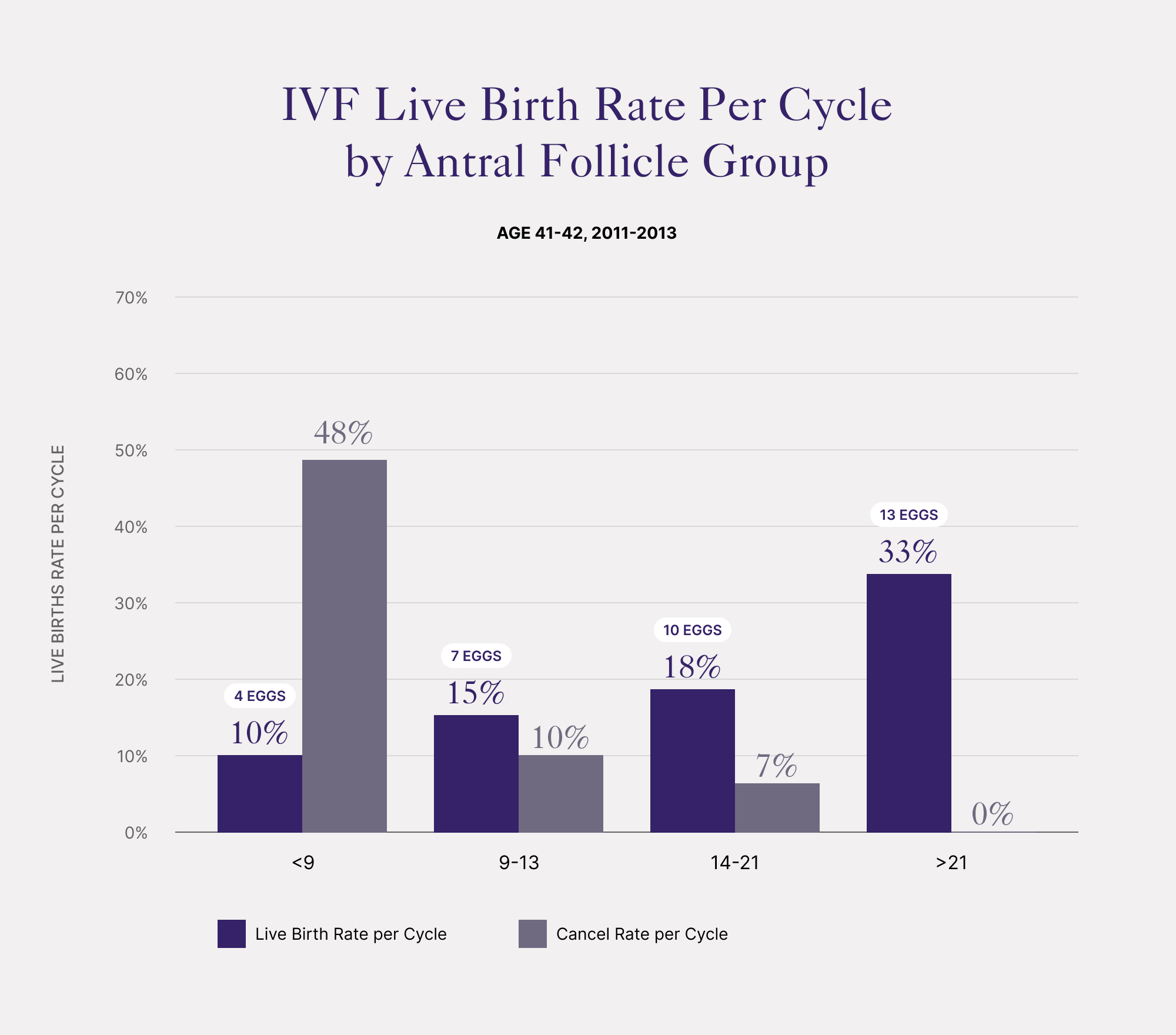
As shown below, there is a strong association between antral numbers and:
- Ovarian response to stimulating medications
- Chances for IVF success
- Risk of having a canceled cycle
The association between success rates and female age is obvious. Most of the decline with advancing age is due to increasing rates of chromosomal abnormalities in older eggs.
- Some couples have their embryos screened for chromosomal errors with PGS, preimplantation genetic screening
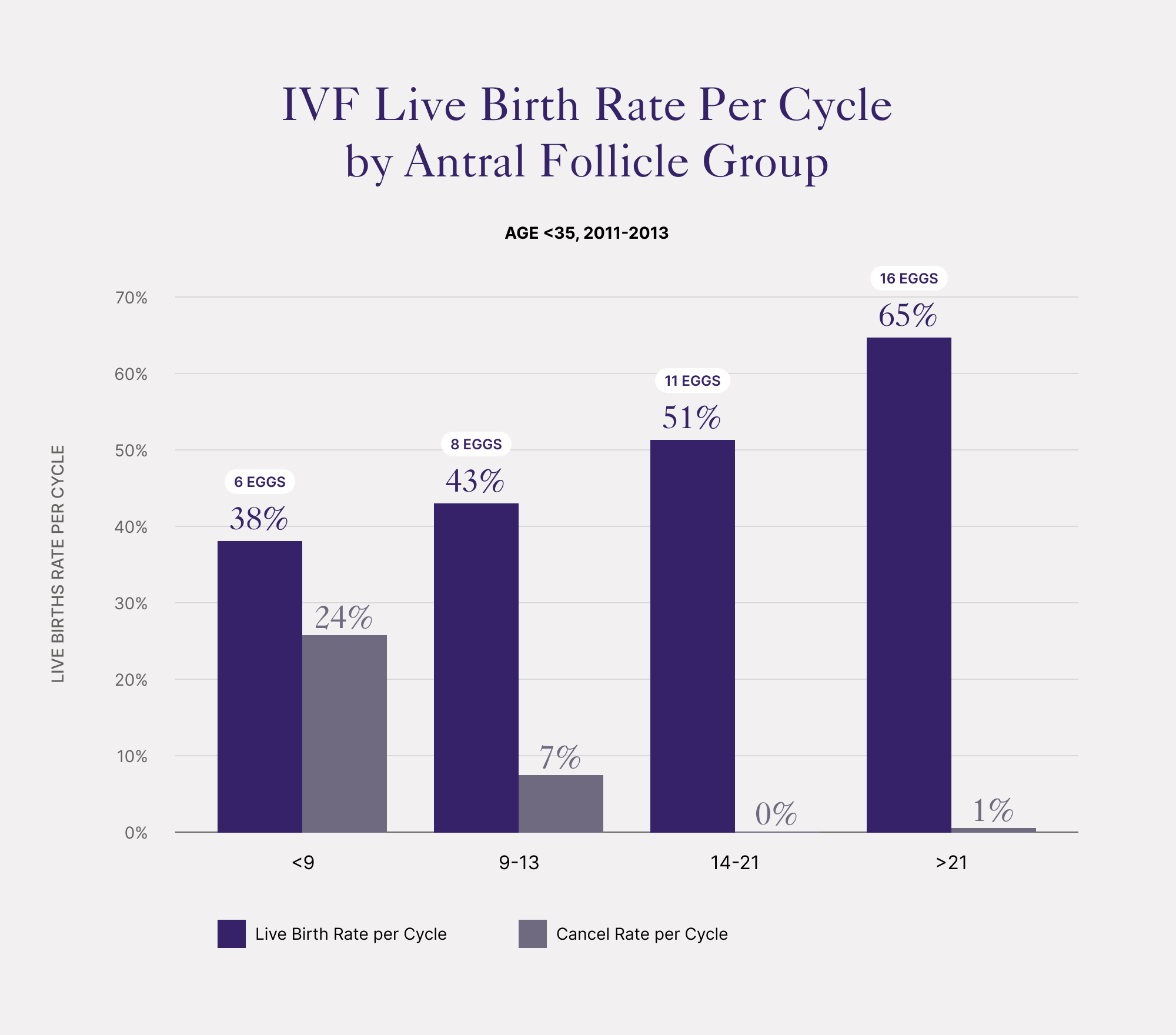
In the charts below:
- Live birth success rates shown by blue columns
- Rate of IVF cycle cancellation before egg retrieval shown by orange columns
- Average number of eggs retrieved shown in red text
IVF success by antral count under 35 years old
Antrals and IVF Success for Female Age Under 35 at Advanced Fertility Center of Chicago
IVF live birth rates are reduced with low antral follicle counts Women with low antral counts give fewer eggs and have higher cycle cancellation rates The median antral follicle count in women under age 35 age was 20 IVF success and cancellation rates by antrals at age 35 to 37.
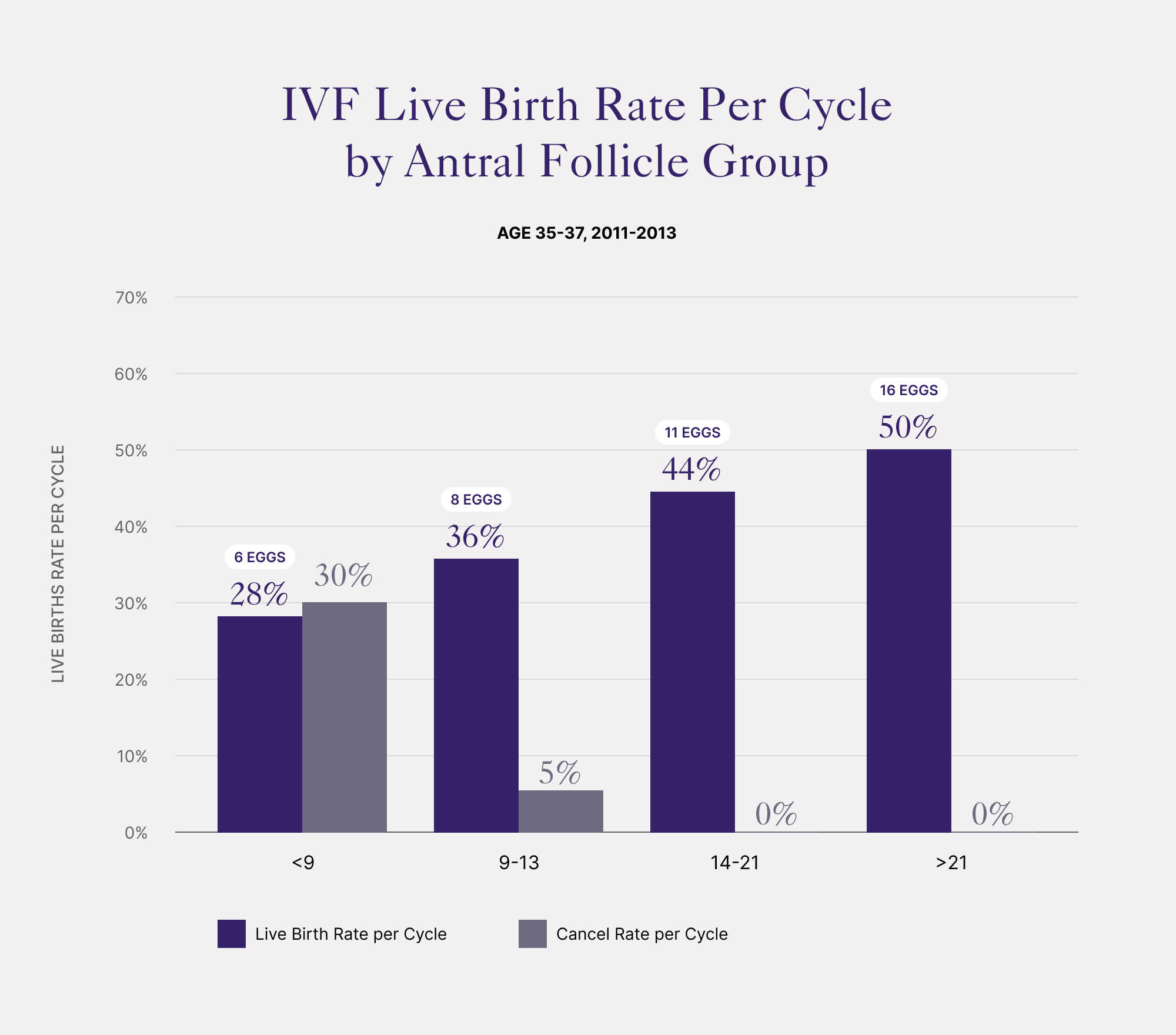
Antrals and IVF Success for Female Age 35-37 at Advanced Fertility Center of Chicago
Women 35 to 37 years old have slightly lower success than the younger women. Slightly higher rates of cycle cancellation are also seen. The median antral follicle count at age 35-37 was 17 Age 38-40 antral follicle counts and IVF success.
Antrals and IVF Success for Female Age 38-40 at Advanced Fertility Center of Chicago
The median antral follicle count at age 38 to 40 was 13 Age 41 to 42 IVF outcome by antral follicles.
Antrals and IVF Success for Female Age 41-42 at Advanced Fertility Center of Chicago
Women age 41 to 42 have substantially lower success rates Having high antral counts improves success rates more at this age The median count at this age was only 11 The above data is from our IVF program at the Advanced Fertility Center of Chicago.
Ready for an Appointment in the Chicago Area?
If you’re ready to explore treatment, contact the award-winning team at AFCC.
Find a Prelude Fertility Clinic Location Near You
The Prelude Network is the fastest-growing network of fertility centers in North America.
Risk for cycle cancellation according to the antral count
As seen in the above charts, the chance of “cancellation” when attempting in vitro fertilization is higher with low antral follicle counts. IVF attempts are sometimes “canceled” when the ovaries respond very poorly to stimulation meds. This is because success rates are very low when less than 3 mature follicles are present on ultrasound.
Response to stimulation with gonadotropins (FSH drugs)
The level of response of the ovaries when the woman takes injectable FSH for stimulation is often predictive of the egg quantity and quality – and therefore, also the relative chances for success with infertility treatment. The level of response that we will get from ovarian stimulating drugs can be estimated in advance with antral follicle counts (see above table). There are no absolute and accepted cutoffs for defining “low”, “normal”, or “high-responders”. However, here are some guidelines.
Low responder:
- When stimulated aggressively with injectable FSH will develop less than 5 mature follicles – often requiring high doses of the medications
- Some women will only develop 1 or 2 mature follicles – even on high drug doses
- These women might not be good candidates for IVF using their own eggs and could possibly need IVF with donor eggs
“Normal” or “average” responder
- When stimulated aggressively with injectable FSH will develop 5-8 mature follicles as well as several smaller ones
High responder: - When stimulated with injectables can develop about 8 or more mature follicles as well as many small and medium-sized follicles
- These women usually respond briskly to lower doses of medications
- They are at higher risk for ovarian hyperstimulation syndrome unless a Lupron trigger is used
In vitro fertilization is a treatment for infertility and is not done as a “test”, but it does give us some information about egg and embryo quality.
- Careful examination of the eggs and embryos during the in vitro incubation process in the laboratory can give us clues about “egg quality”
- For example, eggs may demonstrate poor morphology, may have problems with maturation, or with fertilization, proper cleavage, or blastocyst formation, etc.