A hysterosalpingogram (HSG) is a fertility test used to assess tubal patency and the normalcy of the uterine cavity.
What is a Hysterosalpingogram?
A hysterosalpingogram, or HSG is an important test of female fertility potential. The HSG test is a radiology procedure usually done in the radiology department of a hospital or outpatient radiology facility.
- Radiographic contrast (dye) is injected into the uterine cavity through the vagina and cervix
- The uterine cavity fills with dye and if the fallopian tubes are open, dye fills the tubes and spills into the abdominal cavity
This shows whether the fallopian tubes are open or blocked and whether a blockage is at the junction of the tube and uterus (proximal) or at the other end of the tube (distal).
- Successful treatment for tubal factor infertility is available
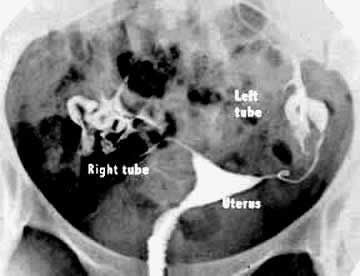
Normal HSG
A smooth triangular uterine cavity and spill from both tubes The bones of the pelvis are seen on the x-ray around edges of image
HSG with blocked tubes
HSG showing a normal uterus and blocked tubes No “spill” of dye is seen at the ends of the tubes Both tubes are slightly dilated and fluid filled – hydrosalpinx This woman went on to have successful in vitro fertilization for her tubal infertility.
What else can be seen by a hysterosalpingogram, besides whether the tubes are open?
Other things that can be seen on a hysterosalpingogram include:
- The uterine cavity is evaluated for the presence of congenital uterine anomalies, polyps, fibroid tumors or uterine scar tissue
- The fallopian tubes are also examined for defects within them, for suggestion of partial blockage, and for evidence of pelvic scar tissue in the abdominal cavity near the tube
What to Expect During a Hysterosalpingogram
The hysterosalpingogram study only takes about 5 minutes to perform. However, the test is usually done in the radiology department of a hospital so there is additional time for the woman to register at the facility and fill out a questionnaire and answer questions regarding allergies to medication etc. The way the test is done is the following:
- The woman lies on the table on her back and brings her feet up into a “frog leg” position.
- The doctor places a speculum in the vagina and visualizes the cervix.
- Either a soft, thin catheter is placed through the cervical opening into the uterine cavity or an instrument called a tenaculum is placed on the cervix and then a narrow metal cannula is inserted through the cervical opening.
- Contrast is slowly injected through the cannula or catheter into the uterine cavity. An x-ray picture is taken as the uterine cavity is filling and then additional contrast is injected so that the tubes should fill and begin to spill into the abdominal cavity.
- More x-ray pictures are taken as this “fill and spill” occurs. When both tubes spill dye, the woman is often asked to roll to one side or the other slightly to give a slightly oblique x-ray image which can further delineate the anatomy.
- The procedure is now complete. The instruments are removed from the cervix and vagina.
- The woman usually remains on the table for a few minutes to recover from the cramping caused by injection of the contrast.
- The results of the test can be immediately available. The x-ray pictures can usually be reviewed with the woman several minutes after the procedure is done.
Can HSG Improve the Chance for Getting Pregnant?
Pregnancy rates in several studies have been reported to be very slightly increased in the first months following a hysterosalpingogram. This could be to the flushing of the tubes opening a minor blockage or cleaning out some debris that was preventing the couple from conceiving.
Some studies suggest that using oil based contrast provides a slightly larger increase in pregnancy success rates than the use of water based contrast. However, the large majority of HSGs are done with water based contrast.
Complications
Complications associated with a hysterosalpingogram include the possibility of an allergic reaction to the dye, which is uncommon. This usually causes a rash, but can rarely be more serious. Pelvic infection or uterine perforation are also possible complications, but these are very uncommon.
If a woman has multiple sexual partners or is otherwise at risk for sexually transmitted diseases, she might be screened with cervical cultures before doing an HSG. Some physicians prescribe several days of antibiotics to reduce risk of infection after HSG.
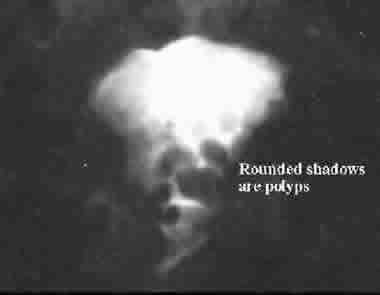
HSG showing multiple “filling defects” in uterine cavity These represent numerous endometrial polyps The polyps were then removed by hysteroscopic resection
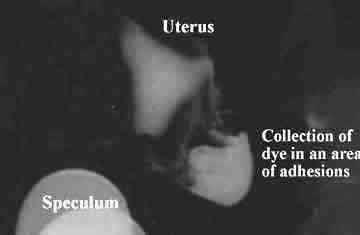
Abnormal study with a collection of dye in a “pocket” at the end of the left tube Scar tissue (adhesions) are holding the dye in the pocket Right tube was previously removed at surgery for a tubal pregnancy
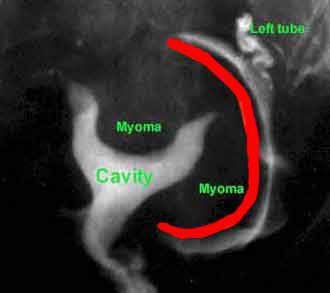
Hysterosalpingogram picture showing uterus with a fibroid that is pushing in to the cavity Another fibroid on the outside of the uterus is circumscribed by dye along the red line Fibroids inside the cavity can cause infertility, miscarriage or preterm birth