Asherman’s Syndrome: Causes, Symptoms, Diagnosis & Treatment
What Are Intrauterine Adhesions?
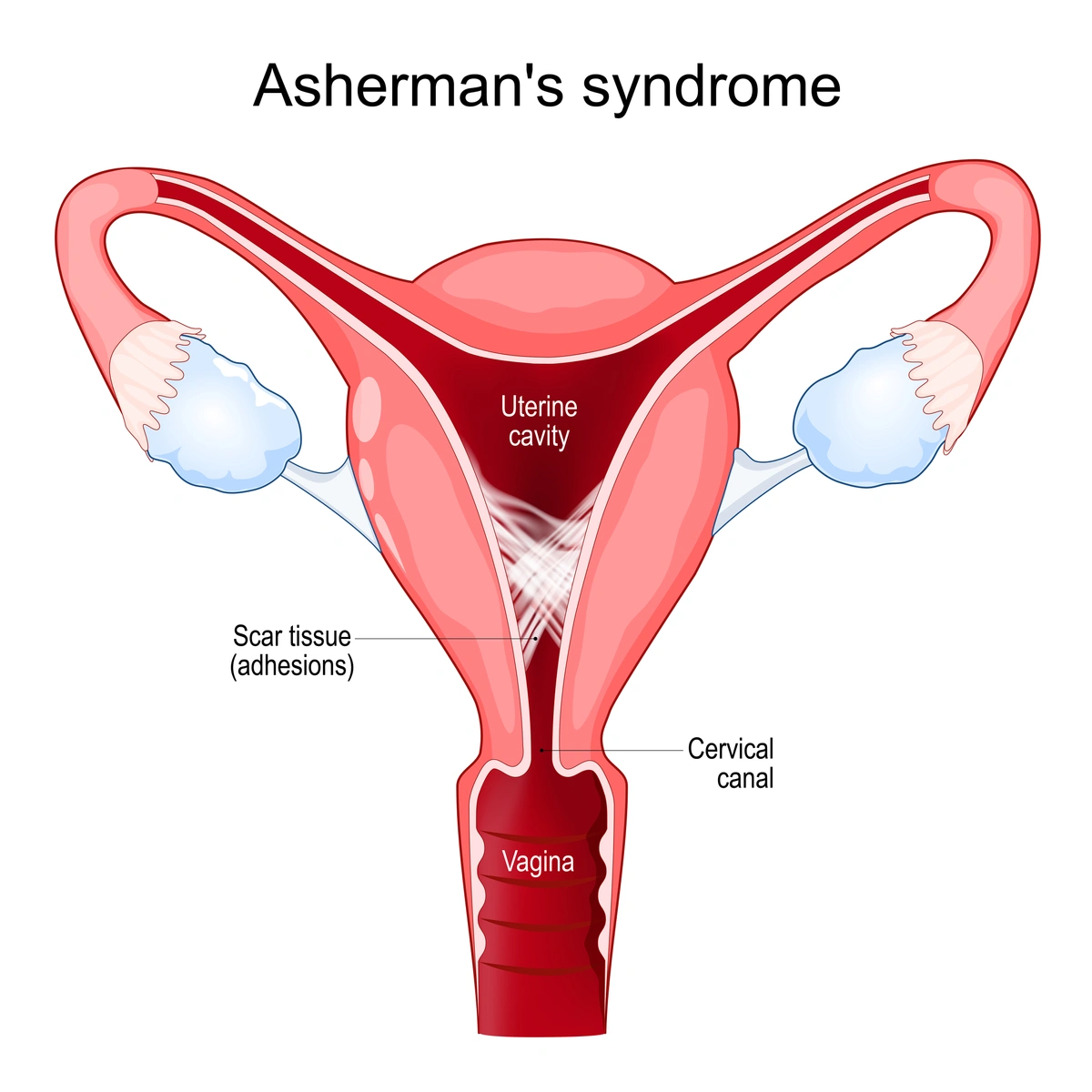
Intrauterine adhesions (IUAs) are bands of scar tissue that form inside the uterus, often as a result of trauma or surgical procedures. When these adhesions become extensive and cause partial or complete blockage of the uterine cavity, the condition is known as Asherman’s Syndrome.
This condition can disrupt the normal function of the uterus and lead to menstrual abnormalities, recurrent pregnancy loss, infertility, and pregnancy and delivery complications. Fortunately, with timely diagnosis and expert treatment, many women can recover normal uterine function and go on to conceive successfully.
Illustration of uterine adhesions
What Causes Asherman’s Syndrome?
The most common cause of intrauterine adhesions is uterine trauma, especially following procedures such as:
-
Dilation and Curettage (D&C): Often performed after miscarriage, abortion, or retained placenta from a live birth
-
Cesarean section (C-section): Particularly if complications such as severe infection occur
-
Myomectomy or fibroid removal surgeries
-
Endometrial ablation: A procedure to treat heavy menstrual bleeding
-
Pelvic infections: Such as tuberculosis or severe endometritis (although these are rare in the U.S.)
Notably, the risk increases with repeated procedures or when surgery is performed after pregnancy, when the uterine lining is especially fragile.
Symptoms of Intrauterine Adhesions
Symptoms can range from mild to severe depending on the extent and location of the adhesions. Common signs include:
-
Light or absent menstrual periods (amenorrhea or hypomenorrhea)
-
Painful menstrual cramping without bleeding
-
Recurrent miscarriage or infertility
-
Difficulty with embryo implantation during IVF
-
Placental abnormalities (in future pregnancies)
Some women have no obvious symptoms and only discover the condition during fertility evaluation or recurrent pregnancy loss testing.
How Are Intrauterine Adhesions Diagnosed?
A thorough evaluation by a fertility specialist is critical. Diagnostic tools may include:
1. Hysteroscopy
A hysteroscopy is the gold standard for diagnosing adhesions. A thin camera is inserted into the uterus to visualize scar tissue directly and assess severity.
2. Hysterosalpingogram (HSG)
An X-ray with dye is used to outline the uterine cavity and fallopian tubes. Adhesions may appear as irregularities or blocked areas.
3. Saline Sonohysterogram (SHG)
Saline is infused into the uterus during an ultrasound. This provides a clearer view of any distorted or collapsed areas within the cavity.
Treatment: Restoring the Uterine Cavity
Most cases of intrauterine adhesions are treatable with minimally invasive surgery, especially when caught early.
Hysteroscopic Adhesiolysis
A fertility specialist uses a hysteroscope to carefully cut and remove scar tissue inside the uterus. Microsurgical tools or lasers may be used to minimize damage to surrounding tissue.
Post-Surgical Care to Prevent Recurrence
-
Intrauterine balloon or stent: Keeps the walls of the uterus separated during healing.
-
Estrogen therapy: Encourages regrowth of healthy endometrial tissue.
-
Antibiotics: May be prescribed if infection is a concern.
-
Second-look hysteroscopy: Often performed a few weeks later to ensure that adhesions haven’t reformed.
How Do Intrauterine Adhesions Affect Fertility?
Scar tissue can interfere with embryo implantation, prevent normal menstrual shedding, or increase the risk of miscarriage and placental issues. The impact on fertility depends on the severity and extent of adhesions. Mild adhesions often resolve with a single procedure and have excellent fertility outcomes, while moderate to severe adhesions may require multiple treatments and carry higher risk for pregnancy complications.
With proper diagnosis and treatment, up to 70–80% of women with mild to moderate Asherman’s syndrome can achieve a healthy pregnancy.
Pregnancy After Treatment: What to Expect
Women who conceive after adhesiolysis are monitored closely. Possible risks include:
-
Placenta previa (when the placenta covers part or all of the cervix) or accreta (when the placenta grows too deeply into the wall of the uterus and doesn’t detach properly after birth)
-
Preterm labor
-
Uterine rupture (rare but serious in cases of extensive scarring)
A personalized care plan, including high-risk pregnancy monitoring, is often recommended.
When to See a Fertility Specialist
You should consider evaluation for intrauterine adhesions if you:
-
Have had one or more D&Cs, particularly after pregnancy
-
Experience light or absent periods post-surgery
-
Are trying to conceive with no success
-
Have recurrent pregnancy loss with no clear cause
-
Encounter unexplained failed IVF cycles
Expert Care for Asherman’s Syndrome at AFCC
At Advanced Fertility Center of Chicago, our team specializes in diagnosing and treating intrauterine adhesions using state-of-the-art hysteroscopic techniques. We tailor each treatment plan to support your fertility goals and give you the best chance for a successful pregnancy.
Call us at (847) 662-1818 or request a consultation today!
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.