Fertility Testing: What to Expect and How It Can Help You on Your Journey
If you’ve been trying to conceive without success, or if you’re just beginning to wonder about your fertility health, you might be hearing more and more about fertility testing. Maybe it feels intimidating—or like it’s too soon. But fertility testing isn’t just for those far into the journey. In fact, it’s one of the most empowering first steps you can take.
In this blog, we’ll break down what fertility testing involves, what it can tell you, and why it’s often the key to getting answers, clarity, and confidence—no matter where you are in the process.
What Is Fertility Testing?
Fertility testing is a series of tests—usually for both partners (if applicable)—that help identify potential reasons why getting pregnant may be difficult or delayed. Think of it as a fertility check-up. It provides a clearer picture of how your body is functioning and helps guide next steps, whether that’s continuing to try naturally, making lifestyle changes, or exploring fertility treatments.You may also hear providers refer to fertility testing as a fertility workup or diagnostic testing.
Core Fertility Testing: What to Expect
Most people will start with these foundational tests:
1. Initial Consultation
You’ll meet with a fertility specialist to review your medical history, lifestyle, and reproductive goals. This conversation helps tailor the testing to your needs.
2. Hormone & Blood Tests
These usually happen early in your cycle (days 2–4) and check levels of hormones like:
-
AMH (Anti-Müllerian Hormone): Estimates ovarian reserve.
-
FSH (Follicle Stimulating Hormone) and LH (Luteinizing Hormone): Involved in egg development and ovulation.
-
Estradiol: A form of estrogen that helps evaluate egg quality.
-
TSH (Thyroid Stimulating Hormone) and Prolactin: Assess thyroid and pituitary function.
3. Pelvic Ultrasound
This imaging test allows your provider to assess the health of your ovaries and uterus, and check for conditions like fibroids or ovarian cysts.
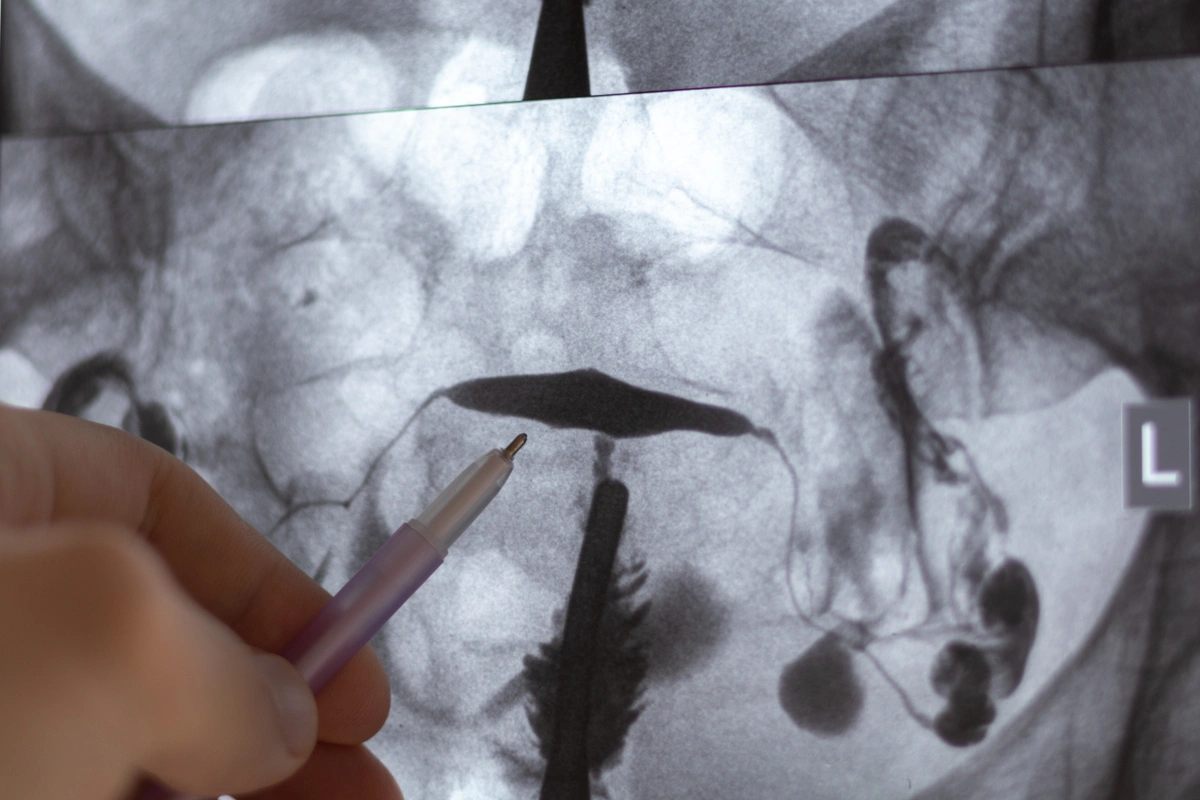
4. HSG (Hysterosalpingogram)
This X-ray evaluates whether your fallopian tubes are open and whether the uterine cavity has any abnormalities that could impact implantation.
Doctor examining X-ray image of Hysterosalpingography (HSG)
5. Semen Analysis
For male partners, this test evaluates:
-
Sperm count (concentration)
-
Motility (movement)
-
Morphology (shape)
Since male factor infertility plays a role in up to 50% of cases, this is a crucial step.
Additional Fertility Tests: When You Need a Deeper Look
In some cases—especially when results are unclear or a more complex history is involved—your provider may recommend more in-depth testing. These can offer even more insight into your reproductive health:
Progesterone Test (Mid-Luteal Phase Test)
-
Why it matters: Confirms if ovulation occurred and whether progesterone levels are high enough to support implantation.
-
When it’s done: Typically 7 days after ovulation, often around day 21 in a 28-day cycle.
Genetic Carrier Screening
-
Why it matters: Screens for inherited genetic conditions (like cystic fibrosis or Tay-Sachs) that could be passed to a child.
-
When it's used: Often done before IVF or if there's a family history of genetic illness.
Karyotype Testing
-
Why it matters: Looks for chromosomal abnormalities that may affect fertility or cause recurrent miscarriage.
-
When it's used: Often recommended for couples with repeated pregnancy loss or unexplained infertility.
Endometrial Biopsy
-
Why it matters: Assesses the health of the uterine lining and checks for inflammation or chronic endometritis.
-
When it's used: In cases of implantation failure, irregular bleeding, or suspected uterine infection.
Sonohysterogram (Saline Infusion Sonogram)
-
Why it matters: A saline-filled ultrasound that offers a clearer look at the inside of the uterus. It’s used to detect polyps, fibroids, or scarring.
-
Alternative to: HSG, especially when uterine structure is a concern.
Full Thyroid Panel & Anti-Thyroid Antibodies
-
Why it matters: Thyroid imbalances can interfere with ovulation and increase miscarriage risk.
-
Includes: TSH, Free T4, and thyroid antibodies to detect autoimmune thyroid conditions like Hashimoto’s.
Prolactin Level
-
Why it matters: Elevated prolactin can suppress ovulation and lead to irregular cycles.
Vitamin D and Nutrient Panels
-
Why it matters: Low levels of certain vitamins (especially Vitamin D, B12, iron, and folate) can negatively impact reproductive hormones, egg quality, and implantation.
Pelvic MRI
-
Why it matters: Offers a detailed view of the uterus and pelvic structures, especially useful in diagnosing adenomyosis, deep fibroids, or congenital uterine anomalies.
Sperm DNA Fragmentation Test
-
Why it matters: Assesses sperm DNA quality beyond basic semen analysis. High fragmentation may contribute to failed implantation, IVF failure, or recurrent loss.
Is It Too Early for Testing?
One of the most common concerns we hear is: “Am I jumping the gun?”
The truth is: you don’t have to wait a year if you have concerns, irregular cycles, or just want more insight into your fertility health. Many people choose to test proactively—just like you’d get your cholesterol or blood pressure checked.
Knowledge is power. And testing is one of the best tools available to make informed decisions.
What Happens After Testing?
Once testing is complete, your provider will walk you through your results and next steps. Depending on what’s discovered, your care plan may include:
-
Continued natural attempts at conception
-
Lifestyle and nutrition changes
-
Ovulation support medications
-
IUI or IVF
-
Egg or sperm preservation
-
Surgical options (if needed)
Whether your results are totally normal, mildly off, or more complex, fertility testing gives you a foundation to build from.
You Don’t Have to Guess Anymore
Fertility testing is about understanding, not labeling. It’s about giving yourself the information you deserve to make the best decisions for your body and future.
At Advanced Fertility Center of Chicago we’re here to support you—wherever you are in your journey.
Want to get a clearer picture of your fertility health?
Schedule a consultation or explore our fertility testing services today. We're here to help you move forward with confidence!
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.