Getting Pregnant After Tubal Ligation: Tubal Reversal vs. IVF
Some women who undergo tubal ligation ("having their tubes tied") later reconsider and hope to grow their families. Fortunately, there are two primary options available for achieving pregnancy after tubal ligation: tubal reversal surgery and in vitro fertilization (IVF). Both approaches have pros and cons, and the right choice depends on several medical and personal factors.
Understanding Your Options
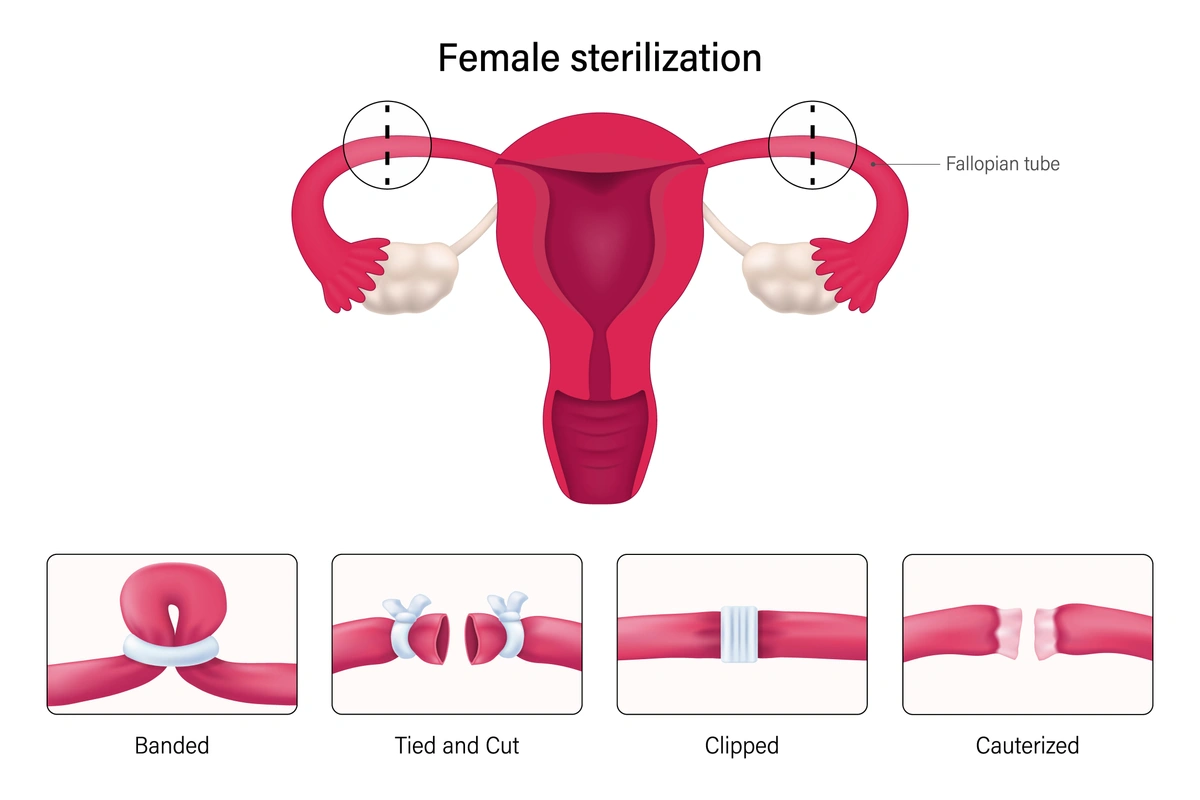
Tubal Reversal Surgery involves reconnecting the fallopian tubes that were previously tied, clipped, or burned. If the surgery is successful, natural conception becomes possible again.
IVF bypasses the fallopian tubes entirely. It involves stimulating the ovaries with medication, retrieving eggs, fertilizing them in the lab with sperm, and transferring resulting embryos directly into the uterus.
Methods of tubal ligation
Key Factors to Consider
1. Sperm Quality
A semen analysis is essential before considering surgery. If the male partner has low sperm count or motility, IVF with ICSI (intracytoplasmic sperm injection) is typically more effective than natural conception after a reversal.
2. Tubal Anatomy
The success of tubal reversal depends on the length and condition of the remaining fallopian tubes. Longer, undamaged tubes (with healthy fimbria) offer better pregnancy chances. Fimbria are the delicate, finger-like projections at the end of the fallopian tubes that help capture the egg after ovulation. Unfortunately, the full condition of the tubes can only be assessed during surgery.
3. Other Pelvic Conditions
Endometriosis or pelvic scar tissue can decrease the likelihood of successful natural conception. IVF is typically more effective for patients with these conditions.
4. Age and Ovarian Reserve
Fertility naturally declines with age, particularly after age 35. By age 43–44, pregnancy success rates for both IVF and tubal reversal drop significantly. Ovarian reserve testing (like AMH level and antral follicle count) helps determine your chances of success.
5. Recovery and Invasiveness
Tubal reversal typically requires abdominal surgery and a longer recovery (up to 3 weeks). IVF is less invasive but involves daily hormone injections and multiple appointments.
6. Future Contraception
If tubal surgery is successful, contraception may be required once the desired number of babies is achieved.
Pros & Cons of Tubal Reversal and IVF
Tubal Reversal – Pros
-
Natural conception is possible: Once healing is complete, you can try to conceive naturally without ongoing medical intervention.
-
One-time procedure: If successful, no additional procedures or medications are needed for future pregnancies.
-
Lower risk of multiple pregnancy: Natural conception has a much lower chance of twins or higher-order multiples compared to IVF, unless you have a family history or specific fertility traits.
-
More affordable long-term for those wanting multiple children: If you plan to have more than one child, reversal may cost less over time compared to undergoing multiple IVF cycles.
Tubal Reversal – Cons
-
Major surgery required: Tubal reversal typically involves a larger abdominal incision and comes with surgical risks such as infection, bleeding, or adverse reactions to anesthesia.
-
Longer recovery time: Patients often need 1 to 3 weeks off work to recover.
-
No guarantee of success: If pregnancy doesn’t occur after the procedure, IVF may still be required later.
-
Increased risk of ectopic pregnancy: Reattachment of the tubes can result in improper implantation, increasing the risk of a dangerous tubal (ectopic) pregnancy.
-
Future contraception required: If you no longer want to conceive after reversal, you'll need to consider permanent or long-term birth control again.
IVF – Pros
-
No surgery required: IVF avoids major abdominal surgery and associated risks.
-
Faster path to pregnancy: You’ll know within about 10 days after embryo transfer whether the cycle was successful.
-
Effective across many fertility challenges: IVF is a viable option for those with additional complications such as poor sperm quality, endometriosis, or diminished ovarian reserve.
-
Control over embryo transfer: IVF allows for single embryo transfer (SET), reducing the risk of multiples while maintaining a high pregnancy success rate.
-
Ability to screen embryos: Optional genetic testing (PGT) can screen for chromosomal abnormalities before transfer.
IVF – Cons
-
More expensive per attempt: Each IVF cycle involves considerable costs, and more than one cycle may be necessary.
-
Medication side effects: Hormone injections can cause temporary side effects such as bloating, mood swings, and ovarian hyperstimulation syndrome (OHSS).
-
Multiple visits and coordination: IVF involves frequent office visits for monitoring and procedures, which can be logistically challenging.
-
Emotional intensity: The IVF process can be emotionally and physically demanding, especially if multiple cycles are needed.
Which Option Is Right for You?
There is no one-size-fits-all answer. The best choice depends on your individual situation, including age, sperm quality, tubal anatomy, fertility history, and personal preferences.
That said, most patients today opt for IVF due to its faster timeline, less invasive approach, and high success rates—especially when time is a factor.
If you’re considering pregnancy after tubal ligation, we’re here to help you weigh your options and choose the best path forward. Contact us today to schedule a consultation with one of our fertility specialists.
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.