Embryo Grading & Screening: What They Mean for Your IVF Journey
When you begin your in vitro fertilization (IVF) journey, you’ll hear terms like embryo grading and preimplantation genetic testing (PGT). These steps are essential for optimizing success rates and ensuring healthy outcomes—but what do they really mean? At Advanced Fertility Center of Chicago (AFCC), we believe informed patients make empowered decisions, and this guide will break down these processes and explain how they work together.
What Is Embryo Grading?
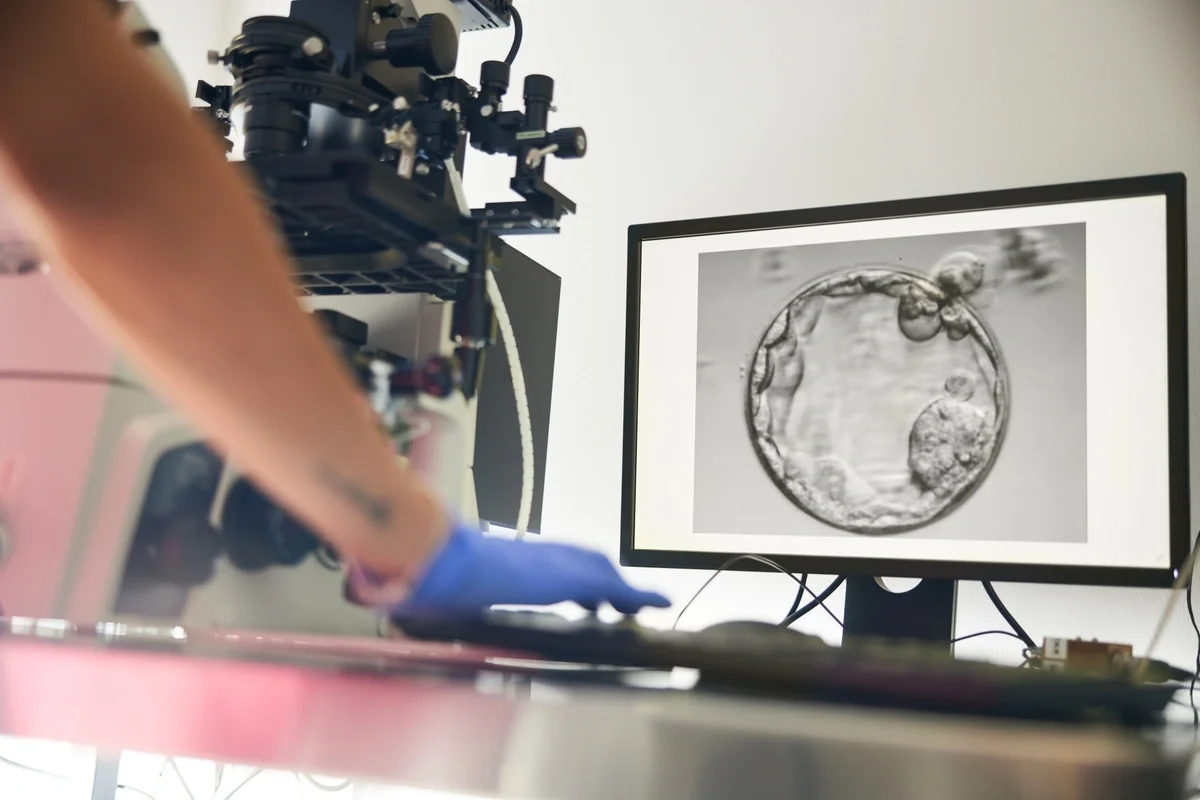
Embryo grading is a visual assessment performed by embryologists under a microscope. It is typically performed once an embryo reaches the blastocyst stage, usually between days 5 and 7 after fertilization in the lab. Embryologists look at factors such as:
-
Cell number and symmetry – Are the cells dividing evenly?
-
Fragmentation – Are there fragments that could affect development?
-
Overall appearance – Does the embryo look healthy and viable?
Why It Matters: Grading helps identify embryos most likely to implant successfully. While it doesn’t guarantee pregnancy, it’s a valuable tool for guiding embryo selection. Our labs in River North and Gurnee use advanced grading systems and prioritize transparency. We explain the “why” behind every recommendation so you feel confident in your choices.
What Do Embryo Grades Measure?
Embryo grades typically reflect:
-
Stage of development (Day 3 cleavage stage vs. Day 5 blastocyst)
-
Cell quality (uniformity and fragmentation)
-
Inner cell mass and trophectoderm quality (for blastocysts)
For example, a Day 5 blastocyst might be graded as 4AA, where:
-
The number (4) indicates expansion stage
-
The first letter (A) reflects inner cell mass quality (A is best)
-
The second letter (A) reflects trophectoderm quality
It’s important to note that grading systems vary by clinic. While most use similar criteria, the scale and terminology can differ.
What If My Embryos Have Different Grades?
It’s common for embryos to have varying grades. A lower grade doesn’t mean an embryo can’t result in a healthy pregnancy. Many successful IVF outcomes come from embryos that weren’t “perfect” on paper. Grading is one piece of the puzzle—not the whole picture.
What Is Preimplantation Genetic Testing (PGT)?
Preimplantation Genetic Testing (PGT) examines embryos for chromosomal abnormalities or specific genetic conditions before transfer. There are different types:
-
PGT-A (Preimplantation Genetic Testing for Aneuploidy): This screens for abnormal numbers of chromosomes (aneuploidy), which can lead to implantation failure or a miscarriage. Key conditions that can be detected with PGT-A include Down syndrome (Trisomy 21) and Turner syndrome (Monosomy X).
-
PGT-M (Preimplantation Genetic Testing for Monogenic Disorders): This detects single-gene disorders in embryos and is often recommended for patients with a known family history of genetic disease. Key conditions that can be detected with PGT-M include cystic fibrosis, sickle cell anemia, Tay-Sachs disease, and Huntington’s disease.
-
PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements): This identifies structural changes in chromosomes, such as translocations or inversions, which can cause infertility or recurrent miscarriage.
What Are the Benefits of PGT?
PGT offers several important advantages for patients undergoing IVF:
-
Improved Implantation Rates: By identifying embryos with the correct number of chromosomes, PGT helps select those most likely to implant successfully, reducing the number of cycles needed to achieve pregnancy.
-
Reduced Risk of Miscarriage: Chromosomal abnormalities are a leading cause of miscarriage. Screening embryos before transfer significantly lowers this risk, offering greater emotional and physical reassurance.
-
Healthier Pregnancy Outcomes: PGT can also detect genetic conditions such as single-gene disorders or structural rearrangements, helping prevent the transmission of inherited diseases and improving the chances of a healthy baby.
-
Personalized Family Planning: For patients with known genetic risks or advanced maternal age, and for patients who prefer family planning, PGT provides critical information to make informed decisions about embryo selection and gender.
-
Cost and Time Efficiency: While PGT adds an upfront cost, it can reduce the need for multiple IVF cycles, saving time, emotional energy, and financial resources in the long run.
-
Peace of Mind: Knowing that embryos have been screened for chromosomal and genetic health offers reassurance during what can be an emotionally challenging journey.
How Grading & Screening Work Together
Embryo grading and genetic screening are complementary tools that provide a more complete picture of embryo health:
Grading Looks at Structure and Development
Embryo grading focuses on visual characteristics—cell symmetry, fragmentation, and overall appearance. It helps embryologists identify embryos that appear strong and viable.
Screening Looks at Chromosomal and Genetic Health
PGT goes deeper, analyzing the embryo’s genetic makeup to detect chromosomal abnormalities or inherited conditions that grading alone cannot reveal.
Why Both Matter
A high-grade embryo may still have chromosomal issues, and a lower-grade embryo can sometimes be genetically normal. Combining both methods allows your care team to select embryos with the best balance of visual quality and genetic health. The combination of grading and screening can improve implantation rates, reduce miscarriage risk, and increase the likelihood of a healthy pregnancy. This integrated approach is especially valuable for patients with advanced maternal age, recurrent pregnancy loss, or known genetic concerns.
At AFCC, these tools are designed to inform—not dictate—your decisions. We provide clear explanations and personalized recommendations so you feel confident and empowered throughout your IVF journey.
Common Questions & Misconceptions
Does a “perfect” grade guarantee pregnancy?
No—grading is predictive, not definitive.
Is genetic screening always necessary?
Not always. It depends on age, medical history, clinical factors, and patient preference.
Will screening harm the embryo?
No. Modern biopsy techniques are safe and widely used.
AFCC’s Patient-Centered Approach
Your IVF journey is emotional, and we’re here to make it as calm and clear as possible. We believe education is empowerment—and we’re committed to guiding you with compassion and expertise.
Ready to Learn More?
Schedule a consultation with AFCC’s fertility specialists today. Let’s take the next step toward building your family—together.
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.

