Understanding Hysteroscopy: A Key Tool in Fertility Evaluation
When navigating the path to parenthood, a thorough investigation of common causes of infertility and miscarriages is paramount. For many patients, especially those facing unexplained infertility or recurrent pregnancy loss, one procedure that can provide both diagnosis and treatment is hysteroscopy.
What Is Hysteroscopy?
Hysteroscopy is a minimally invasive procedure that allows fertility specialists to directly examine the inside of the uterus. Using a thin, lighted telescope called a hysteroscope, the physician inserts the device through the cervix to visualize the uterine cavity in real time. This procedure can be diagnostic (to observe and assess) or operative (to treat abnormal findings).
Image of hysteroscope
Unlike traditional imaging methods like ultrasound or HSG (hysterosalpingogram), hysteroscopy provides a clear, direct view of the uterine cavity, allowing for precise identification—and eventual removal—of abnormalities such as:
-
Polyps
-
Fibroids
-
Scar tissue
-
Congenital anomalies like a uterine septum
Why Is It Used in Fertility Care?
Hysteroscopy is often recommended in the following situations:
-
As a routine part of infertility evaluation (combined, when applicable, by sonohysterogram, an ultrasound-guided test for the fallopian tubes)
-
Patients have experienced recurrent miscarriages or failed IVF cycles
-
There are symptoms like irregular bleeding, pain, or suspected uterine abnormalities by ultrasound
-
Prior to embryo transfer
By identifying and treating these conditions, hysteroscopy can improve the chances of successful implantation and pregnancy and reduce miscarriages. In fact, studies show that correcting uterine issues via hysteroscopy may significantly boost fertility outcomes—especially when used before assisted reproductive treatments like IVF.
What to Expect During the Procedure
Most hysteroscopies are performed in an outpatient setting and take around 1 minute, if they are diagnostic, or 10-20 minutes, if they are operative. Here’s a general overview:
-
Preparation: The cervix may be gently dilated.
-
Visualization: The hysteroscope is inserted, allowing the doctor to inspect the uterine cavity, which is being distended with fluids.
-
Treatment (if needed): If abnormalities are found, small instruments can be used to remove or correct them in a separate session (operative hysteroscopy).
Patients typically experience mild menstrual-like cramping or spotting afterwards, with recovery times ranging from 1-8 hours (primarily to let anesthesia wear off). Most return to normal activities the next day with minor restrictions.
What Can Hysteroscopy Reveal?
Hysteroscopy can uncover conditions that may not appear on other tests, including:
-
Endometrial polyps: Local benign overgrowths of the uterine lining
-
Fibroids: Benign growths of the uterine muscle that may distort the uterine cavity
-
Scar tissue
-
Uterine septum (wall) or other birth defects
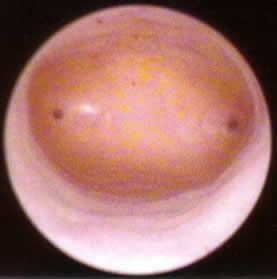
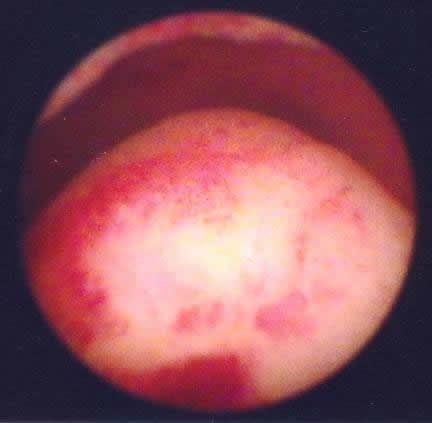
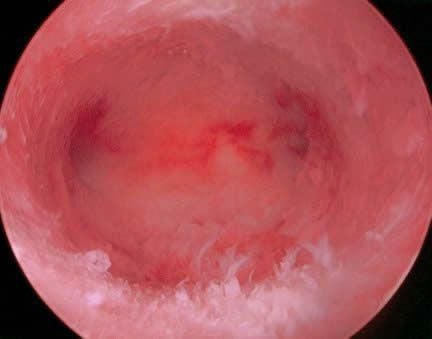
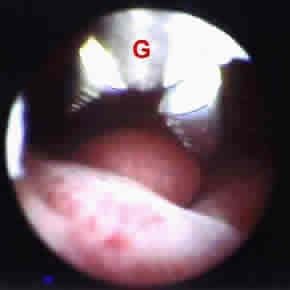
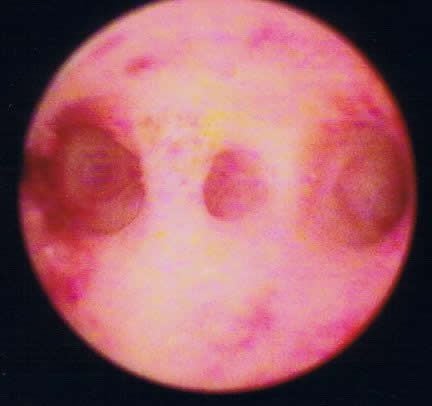
To help patients better understand what hysteroscopy can uncover, we’re including a series of real surgical images from hysteroscopy procedures. These visuals show both normal and abnormal uterine cavities, offering a clear look at what fertility specialists see during the procedure.
Here’s what you’ll find in the image gallery:
-
Normal Uterine Cavity: A healthy uterine lining with visible tubal openings (ostia) on each side.
-
Endometrial Polyps: Bulging tissue (benign excess growth of the uterine lining) that can interfere with implantation—shown before and after removal in images 1 and 2. Image 3 showcases a small polyp being resected with hysteroscopy (grasper at "G").
-
Scar Tissue (when severe - Asherman’s Syndrome): Strands of fibrous tissue that can block embryo attachment. The patient in this image underwent dilation and curettage (D&C) for heavy bleeding following the delivery of a baby.
-
Uterine Septum: A congenital divider in the uterus that may increase miscarriage risk. In the image, the uterine septum is represented by the "S" in middle of picture. The right side of cavity is represented with an "R" and left side with an "L."
-
Fibroids: Uterine muscle-based tumors protruding into the cavity, often resected to restore normal anatomy. In this image, two fibroid tumors are shown bulging down into the endometrial cavity. These fibroids were resected with surgery, resulting in a normal uterine cavity.
These images show how hysteroscopy allows for direct diagnosis and eventual treatment. Whether it’s removing a polyp or correcting a septum, the goal is always the same: to optimize the uterine environment for a healthy pregnancy.
Final Thoughts
Hysteroscopy is more than just a diagnostic tool—it’s a window into the uterine environment and a chance to treat abnormalities if detected. For many patients, it’s the missing piece that brings clarity, confidence, and renewed hope.
If you’re considering fertility treatment and want to learn whether hysteroscopy might be right for you, schedule a consultation with our team today. We’re here to help you move forward—with answers, support, and expert care.
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.